

Journal of Pharmaceutical Research
DOI: 10.18579/jopcr/v20i4.MS21073
Year: 2021, Volume: 20, Issue: 4, Pages: 88-96
Review Article
Suchismita Mishra ✉ 1, Saurav Suman 1, Akshat Gupta 1, Neelima Mishra 1
1 Oriental College of Pharmacy, Oriental Campus, India
✉ Corresponding author: Suchismita Mishra; [email protected]
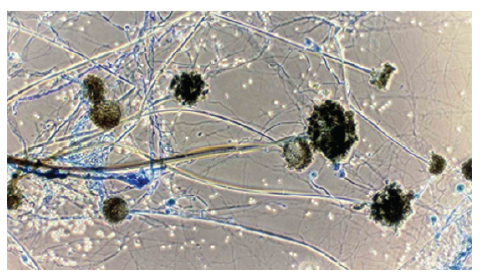
Mucormycosis, also known as Zygomycosis or Black Fungus, is an infection caused in humans via various causative agents from the Zygomycetes class. Several countries including India is afflicted by the covid-19 virus, which has infected approximately 3.7 million people across the country. Some of the corona-positive patients suffer from another fatal infection, Mucormycosis, commonly known as Black Fungus. The strategy should be to administer an effective antifungal drug as soon as possible at the optimum dose. However, India being an epicenter of Diabetes with enormous 80 million diabetics, is of particular importance in the present scenario of the COVID pandemic. COVID therapy with Steroids and immune suppressants has increased the chances of infection in various individuals within the country with weaker immune system responses. The main purpose of this paper is to enlighten the community about the involvement of mucormycosis in covid-19 affected population and basic insights of its invasion.
Keywords
Mucormycosis, Black Fungus, Covid-19, Diabetes Mellitus, Amphotericin B, Immunosuppression, Apophysomyces, Renal Failure, Corticosteroids
© 2021 Published by Krupanidhi Educational Trust. This is an open-access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
Subscribe now for latest articles and news.