

Journal of Pharmaceutical Research
Year: 2024, Volume: 23, Issue: 4, Pages: 226–232
Original Article
Arbind Kumar Chaudhary1,∗, P Feroz Khan2, A Sudhindra Prathap3, Reetesh Kumar Rai4,∗
1Assistant Professor of Pharmacology, Government Erode Medical College and Hospital, Tamil Nadu, India
2Assistant Professor of Anatomy, Government Erode Medical College and Hospital, Tamil Nadu, India
3Tutor, Dept of Pharmacology, SDM college of medical sciences and hospital, Dharwad, Karnataka, India
4Associate Professor, Dept. of Pharmacology, MRA Medical College, Ambedkar Nagar, Uttar Pradesh, India
*Corresponding Author
Email: reetesh3@gmail.com
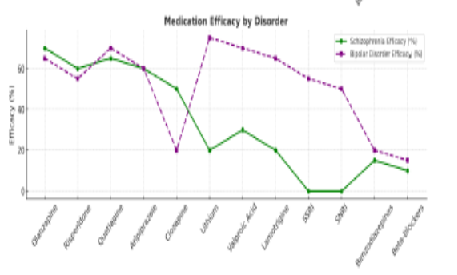
Objective: Objective of the article is to investigate the neurobiological and clinical differences between schizophrenia and bipolar affective disorder, focusing on sociodemographic variables and clinical characteristics. Methods: A cross-sectional study was conducted with 70 patients diagnosed with either schizophrenia (43 patients) or bipolar affective disorder (27 patients). Data were collected on sociodemographic factors, educational background, employment status, socioeconomic status, residential area, and medication adherence. Clinical characteristics, including average age, duration of disease, and duration of exacerbation, were analysed. Chi-square tests were used to assess the significance of differences between the two groups. Results: Schizophrenia patients were predominantly female (57.1%) compared to bipolar disorder patients (42.9%). Educational levels showed that 67.1% of schizophrenia patients had only primary education, while 57.1% of bipolar patients had secondary or higher education. Schizophrenia patients had a higher unemployment rate (22.9%) compared to bipolar patients (14.3%). Socioeconomically, 45.7% of schizophrenia patients were in the low-income bracket versus 22.9% of bipolar patients. Medication adherence revealed that 58.6% of schizophrenia patients used depot medications compared to 18.6% of bipolar patients. Schizophrenia patients had a longer average duration of disease (7.7 years) and exacerbation (12.0 months) compared to bipolar patients (7 years and 6 months, respectively). The study highlights significant sociodemographic and clinical differences between schizophrenia and bipolar affective disorder. Schizophrenia patients tend to have lower educational attainment, higher unemployment rates, and more frequent depot medication usage. They are younger with longer disease duration and exacerbations, while bipolar disorder patients show better educational and employment outcomes and shorter exacerbation periods. Conclusion: These findings underscore the need for tailored treatment approaches and support strategies to address the specific needs of each disorder. Further research is warranted to explore these differences in greater depth and refine therapeutic interventions.
Keywords: Schizophrenia, Bipolar Disorder, Sociodemographic Factors, Clinical Characteristics, Medication Adherence, Neurobiological Differences
© 2024 Published by Krupanidhi College of Pharmacy. This is an open-access article under the CC BY-NC-ND license (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Subscribe now for latest articles and news.